Case Presentation:
Cavernoma, Medullary - Case 1
History & Physical
- 56-year-old right handed lady who presented with nausea and vomiting, difficulty with swallowing, disequilibrium and progressive loss of gait and balance (inability to walk independently). She was also suffering from persistent hiccups and came to the emergency room due to difficulty with breathing.
- Her neurological examination showed complete loss of balance with disequilibrium, dysmetria, dysdiadochokinesis, bilateral Babinski, positive Romberg’s, and dysphonia.
Imaging
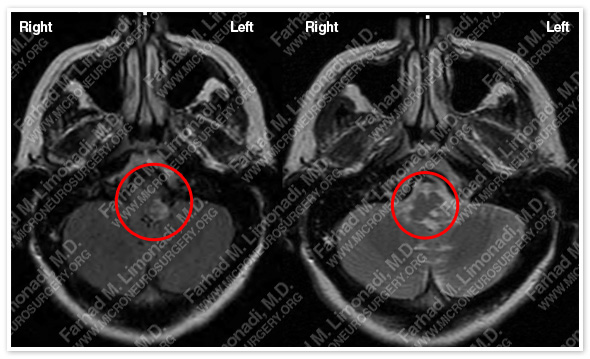
MRI scan of her brain shows a cavernous malformation (cavernoma) arising from the left medullary segment of brain stem with significant mass effect on the brain stem.
MRI at presentation T2 sequence MRI at month later T2 sequence
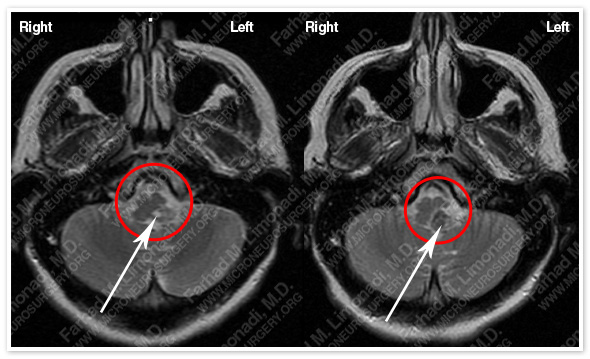
The new MRI showed that the cavernous malformation had re-bled with increasing mass effect on her medulla oblongata (brainstem).
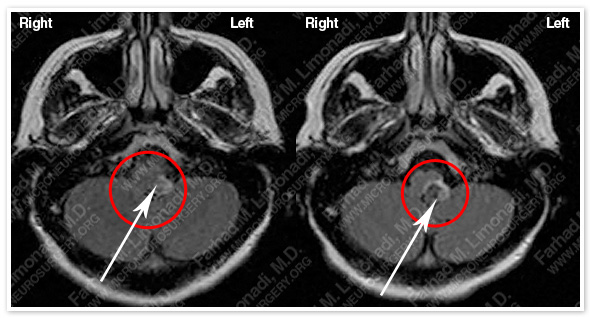
MRI at presentation flair sequence MRI a month later flair sequence
The new MRI showed that the cavernous malformation had re-bled with increasing mass effect on her medulla oblongata (brain stem).
Treatment
- Patient remained stable and given the typical and relative benign course of cavernous malformations and low risk of recurrent hemorrhage, together with the very sensitive location of this lesion (brain stem), patient was managed conservatively initially and eventually discharged home with a plan for radiographic and clinical follow-up.
- However, in less than two weeks she was brought to the emergency room with similar symptoms with progressive difficulty with breathing, and dysphonia.
Computer Navigation

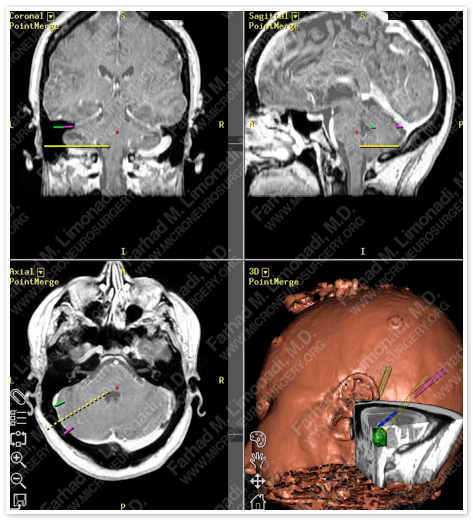
Computer navigation and stereotaxy was utilized to precisely model and map this cavernous malformation for surgical planning. Critical neurovascular structures were individually marked and systematically approached during the operation. Cavernoma is marked in green.
Surgical Procedure
- She underwent left far-lateral skull base craniectomy and surgical resection of this brainstem cavernoma using stereotaxy and brain mapping, intraoperative neurophysiological monitoring including facial nerve monitoring, monitoring of cranial nerves 8, 9, 10, 11, and 12, SSEP, MEP, and brain stem auditory evoked response (BAER).

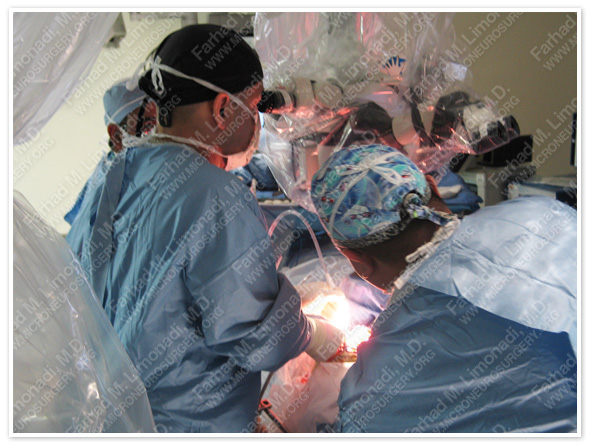
Dr. Limonadi and his team during surgery.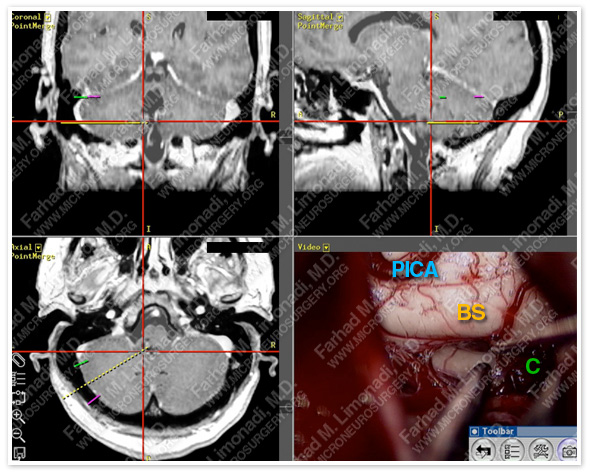
Right lower slide shows the view (through the surgical microscope) of the brain stem posteriorly as the cavernous malformation is being removed.
BS=Brain stem, C=Cavernoma, PICA=Posterior Inferior Cerebral Artery.
This lesion is shown under the hairpin in other slides.
Pathology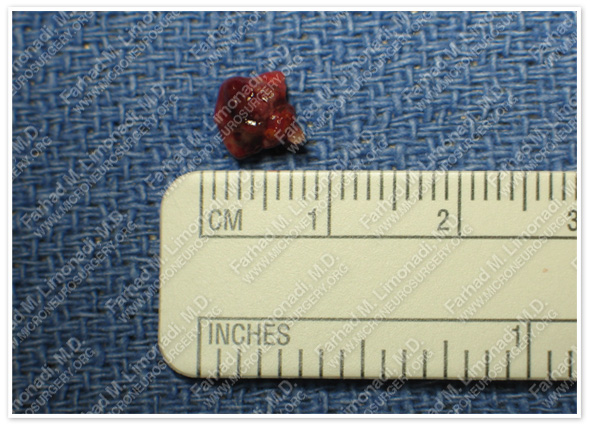
The cavernoma was removed with out any difficulty during surgery and sent for pathological evaluation which confirmed the diagnosis.
Post-op Imaging
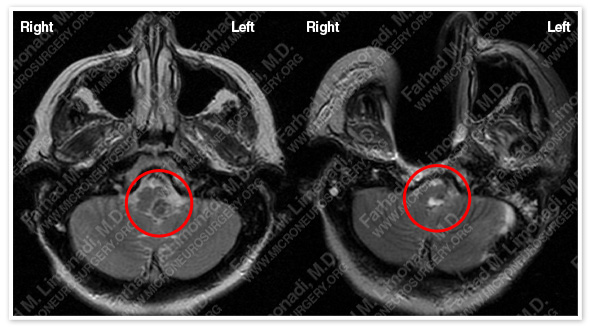
Before Operation After Operation
Post-op MRI shows complete resection of this cavernous malformation without injury to the brain stem (medulla) or adjacent neurovascular structures.
Post-op Course
- She was trached and pegged postoperatively and gradually weaned off both and returned to normal function with regaining her ability to walk and function independently.