Case Presentation:
AVM R Temporal - Case 2
History & Physical
- 50-year-old right handed man who presented with sudden onset of headache and sudden loss of visual field.
- His neurological examination showed right homonymous hemianopsia (loss of vision in right visual field), and upper tract signs in right upper and lower extremities.
Imaging
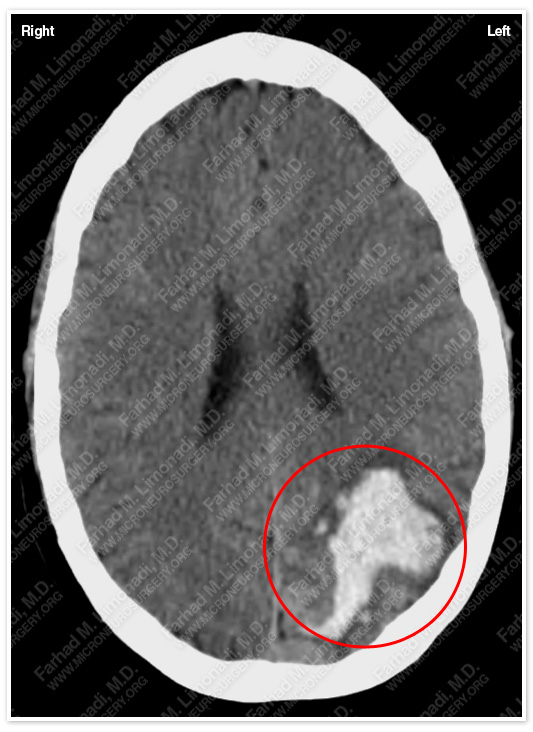
CT scan of his brain shows a left occipitotemporal hemorrhage.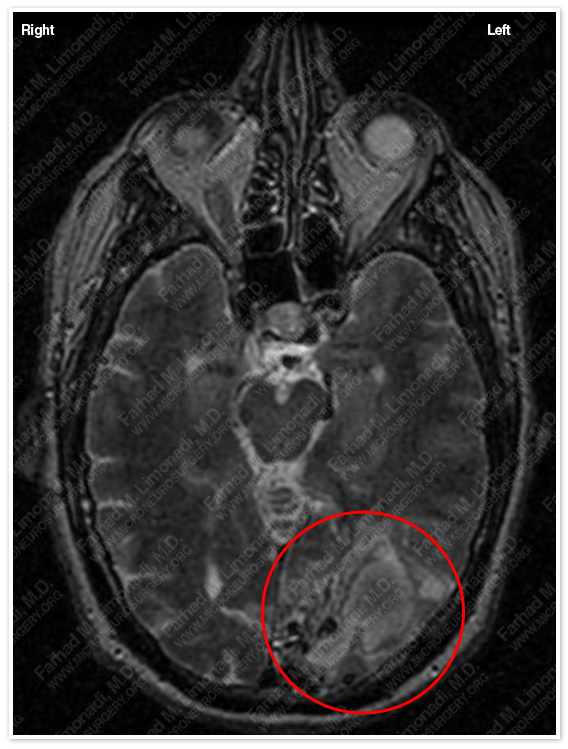
MRI scan of his brain shows the source of this hemorrhage to be a probable arteriovenous malformation (AVM).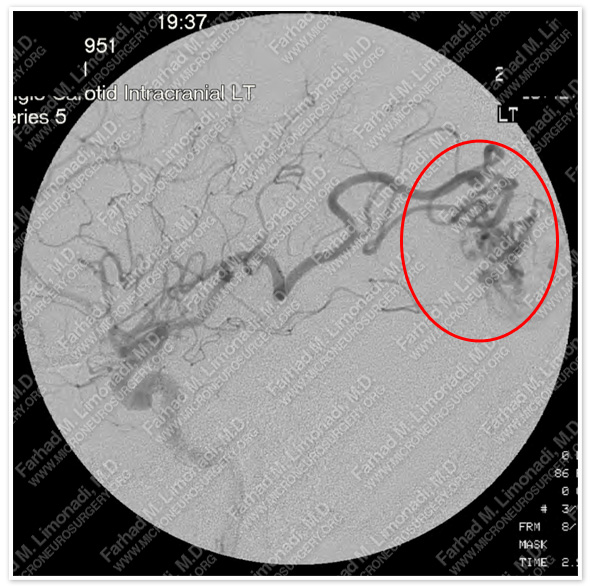
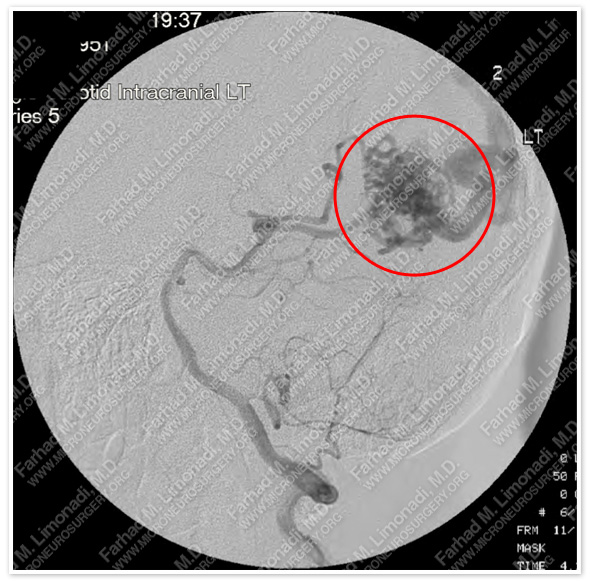
Cerebral angiography confirmed the diagnosis of a complex arteriovenous malformation (AVM) which was supplied by anterior circulation (left slide) and posterior circulation (right slide).
Computer Navigation
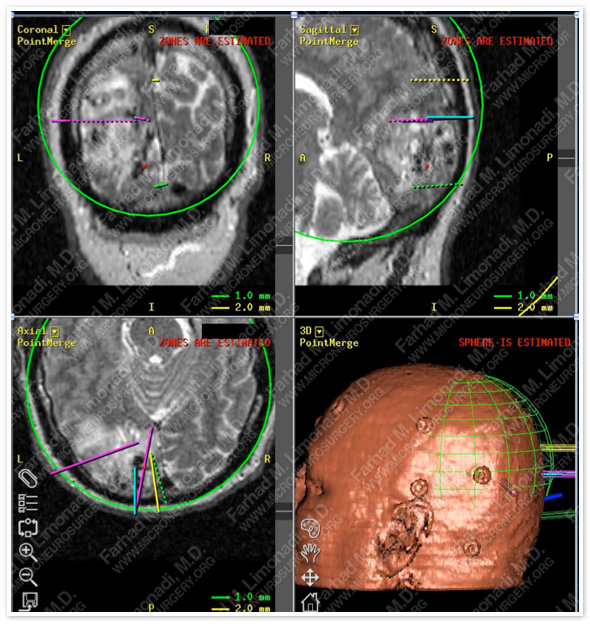
Computer navigation and stereotaxy was utilized to precisely model and map the AVM for surgical planning. Feeding branches were individually marked and systematically approached during the operation.
Surgical Procedure
- He underwent angioembolization of the AVM followed by right occipitotemporal craniotomy using stereotaxy and computer navigation, together with intraoperative neurophysiological monitoring with complete resection of this AVM.
Pathology

The AVM was removed without any difficulty during surgery and sent for pathological evaluation which confirmed the diagnosis.
Post-op Imaging
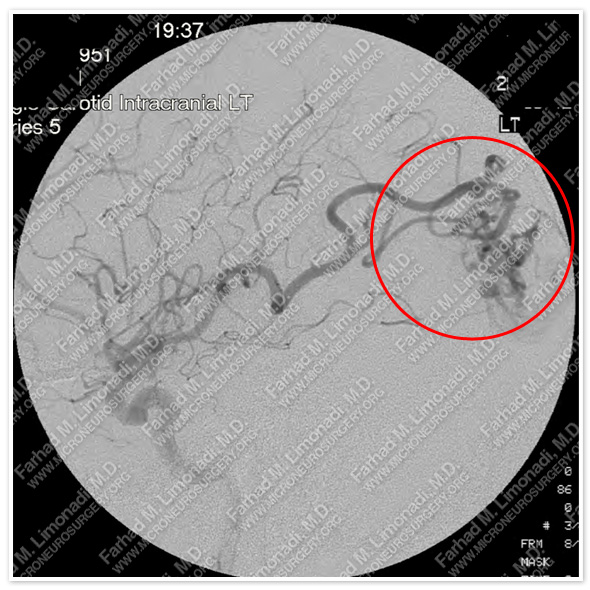
Before Operation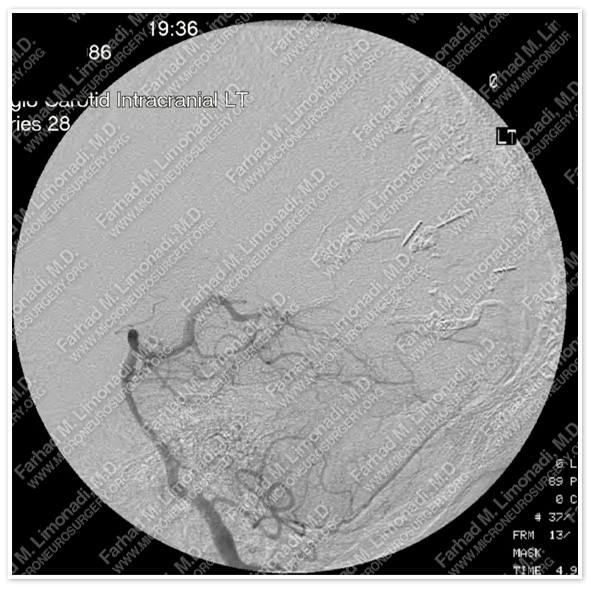
After Operation
Post-op cerebral angiography of anterior circulation shows no residual AVM and intact normal cerebral vasculature.
Post-op Course
- He did well post-operatively with no neurological deficit. His visual field deficit progressively improved. He was discharged home and returned to his home state in good health.