Case Presentation:
Parkinson's Disease - Case 2
History & Physical
- 60+ year-old right handed man with 6+ years history of Parkinson's Disease who initially presented with tremor of right upper extremity which gradually expanded to all extremities. He also developed significant rigidity, bradykinesia, masked facies, and dysautonomia. He was appropriately treated medically with Carbidopa-Levodopa, Mestinon, and Amantadine under supervision of an excellent movement disorder neurologist.
- However, starting 2 years before referral to us he developed significant motor fluctuations and dyskinesia and quite debilitated as the result.
He has significant resting tremor right more than left, as well as masked facies.
- Having failed appropriate conservative medical management by a movement disorder neurologist and developing significant motor fluctuations with dyskinesia, he was considered a good candidate for DBS (Deep Brain Stimulator) implantation with subthalamic nucleus (STN) as an appropriate target.
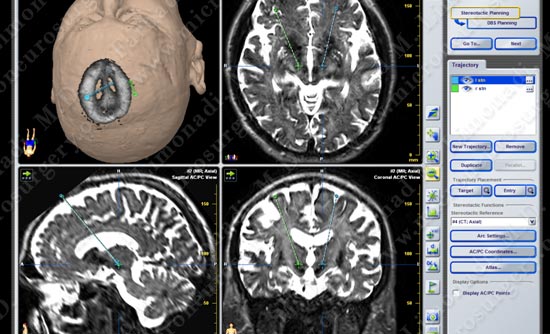 Computer navigation and stereotaxy was utilized to pinpoint the location of the STN on each side with a planned trajectory for implantation of the DBS.
Computer navigation and stereotaxy was utilized to pinpoint the location of the STN on each side with a planned trajectory for implantation of the DBS.

Operating Room

While awake, micro-electrode recording together with stereotaxy is used to pinpoint each subthalamic nucleus (Dr. Limonadi is behind the transparent drape).
Macro-stimulation is used to confirm the target and efficacy of DBS implantation with minimal side effect.
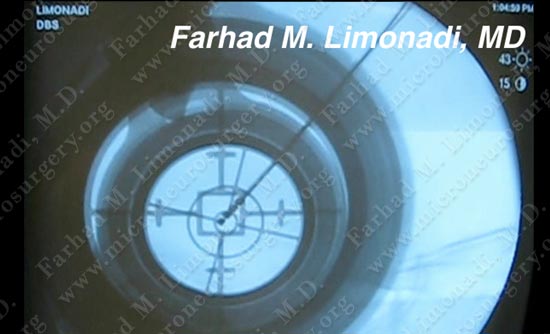
Imaging is also used to confirm proper implantation of each DBS electrode.
Dr. Limonadi examines the patient before concluding the operation.
Post-op Imaging

His tremor, bradykinesia, and masked facies nearly completely resolved post operatively. His quality of life remarkably improved as the result.