Case Presentation:
Craniopharyngioma - Case 1
History & Physical
- 75-year-old gentleman with several episodes of syncope (sudden loss of consciousness), difficulty with gait and balance, and periods of confusion. He had several potential cause including severe COPD with chronic hypoxia, congestive heart failure and cardiac failure, and obesity.
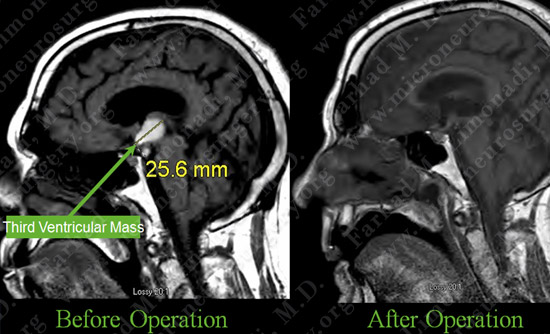
- MRI scan of his brain revealed third ventricular mass within the third ventricle with extension through the floor of the third ventricle and into the peri-mesencephalic cistern.
- On examination he had no focal neurological deficit.
- Given his significant comorbidities and risk factors the decision was made to follow him up radiographically as well as clinically.
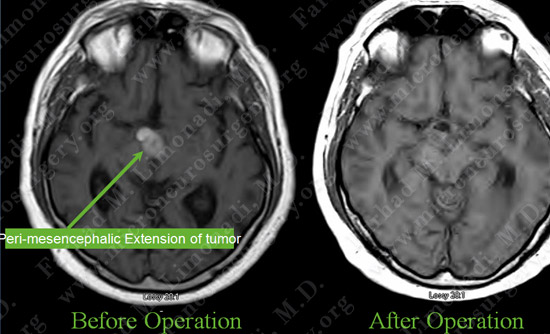
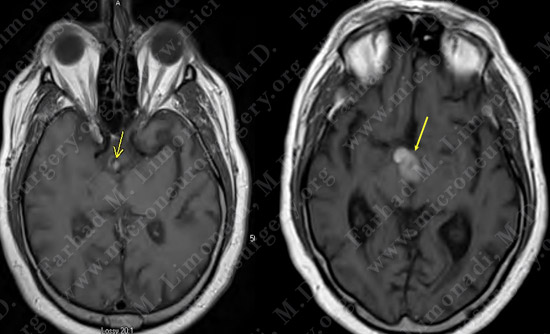
Imaging
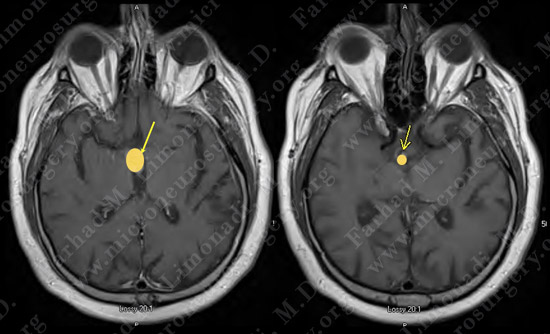
MRI scan of his brain reveals third ventricular mass within the third ventricle (left) with extension through the floor of the third ventricle and into the peri-mesencephalic cistern (right).

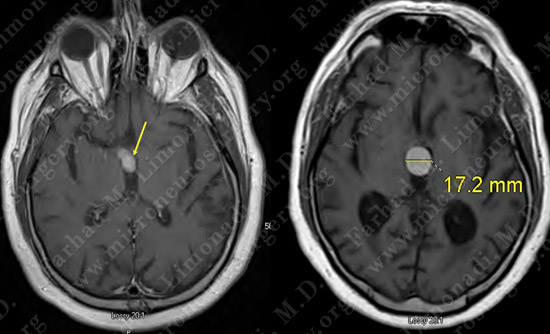
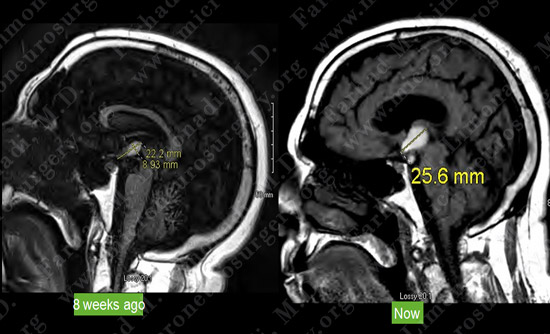
Medical Progress - Imaging
- Within 8 weeks he presented with progressive confusion, and loss of ability to walk.
- MRI scan of his brain revealed significant enlargement of his tumor with more extension through the peri-mesencephalic cistern.
Surgical Procedure
- Given his significant medical co-morbidity's a plan for a minimally invasive surgical approach for resection of his tumor was put in place.
- He underwent a minimally invasive neuro-endoscopic surgery with gross total resection of the tumor, with intra-operative neuro-physiologic monitoring including BAER (Brain Stem Auditory Response), SSEP (Somato-Sensory Evoked Response), MEP (Motor Evoked Response).
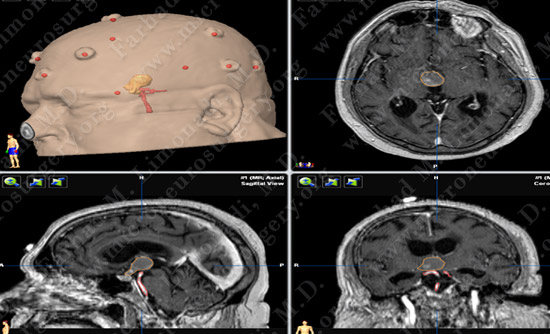
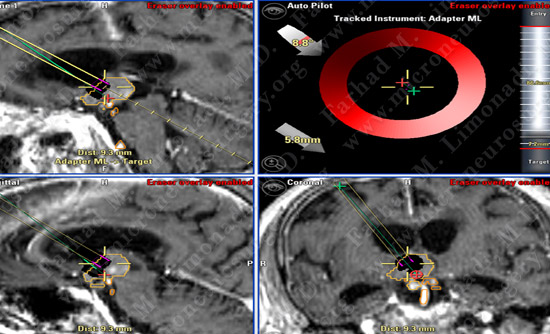
Computer navigation and stereotaxy was utilized to map and localize the tumor (outlined in yellow), and basilar artery and its tributaries (outlined in red) during surgery.
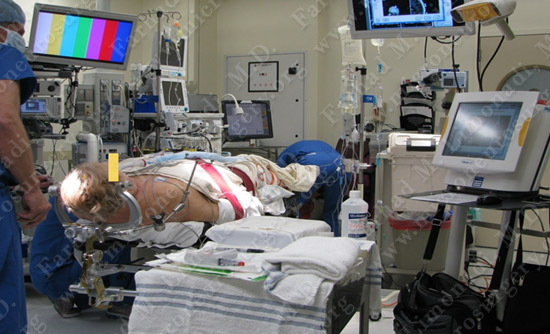
Intra-operative neurophysiological monitoring including Brainstem Auditory Evoked Response (BAER), SSEP and MEP is utilized to monitor his brain functions during the surgery.
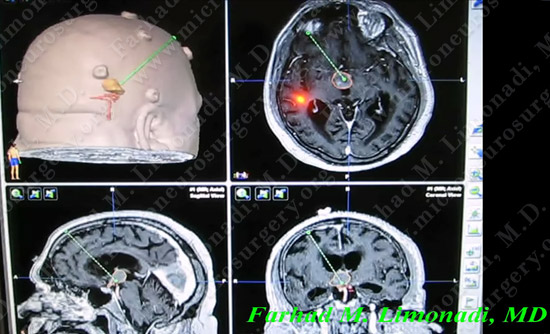
The surgery is simulated using computer navigation: Planned trajectory is colored in green. Tumor is outlined in yellow and basilar artery is outlined in red.
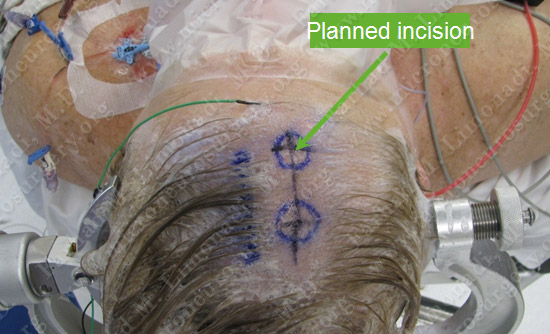
A larger area than normal is shaved in case we have to convert the surgery to open (interhemispheric transcallosal craniotomy). Two separate sites are marked for optimal approach to the tumor.
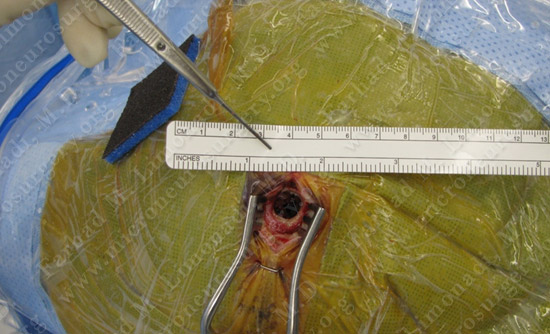
Neuro-endoscope is armed with stereotaxy, and using an incision of approximately 1 inch and a single burr hole (bone opening) with diameter that is smaller than a dime, the endoscope is driven to target using computer navigation and anatomical landmarks.

Dr. Limonadi and his team start to introduce the neuro-endoscope through the small opening and in to the brain. The endoscope is being calibrated.
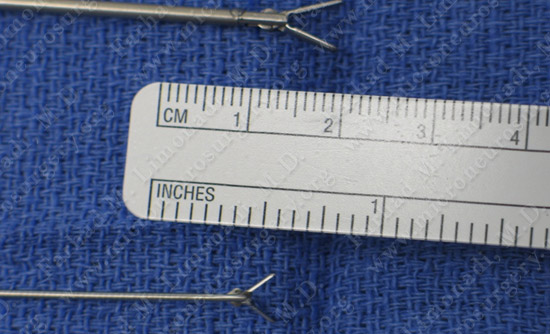
Surgical instruments used through the small working channel of the neuro-endoscope for surgical resection of the tumor.
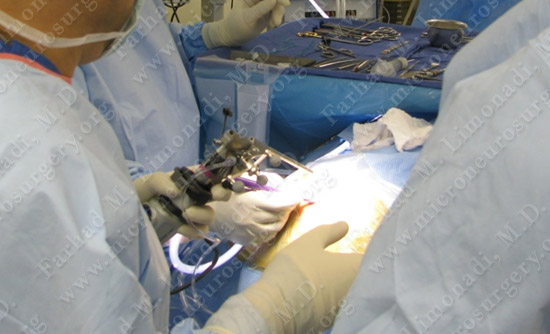
The neuro-endoscope is advanced through the small opening of the skull and in to the brain.
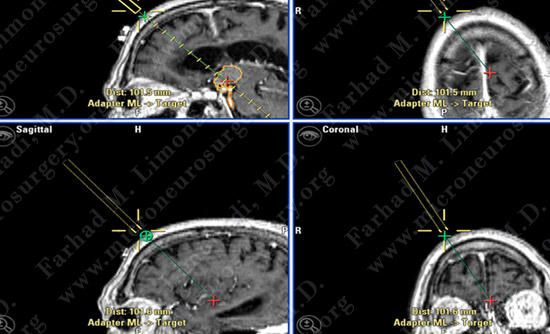
Computer navigation and stereotaxy was utilized to drive the neuro-endoscope (yellow) along the pre-planed trajectory (green) to the tumor (outlined in yellow).
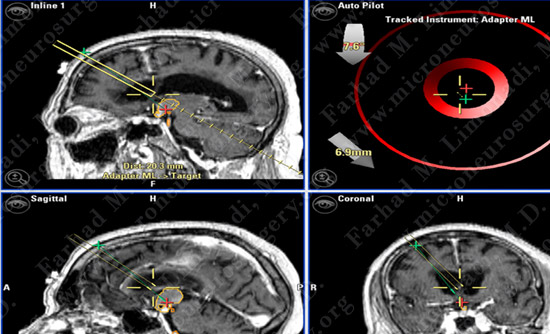
The neuro-endoscope (yellow) is advanced into the frontal horn of the right lateral ventricle along the pre-planed trajectory (green).
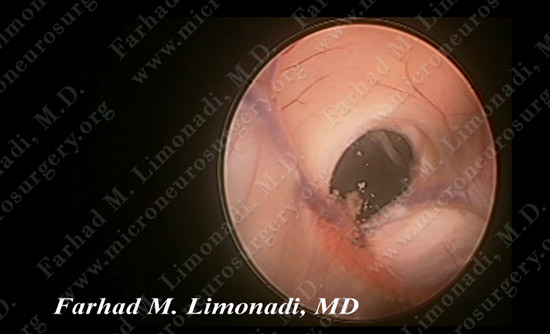
Upon entry into the frontal horn of the right lateral ventricle, import landmarks are identified.
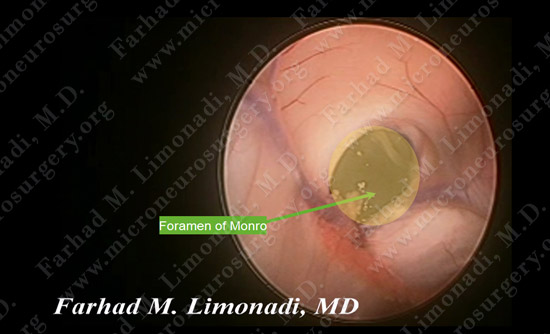
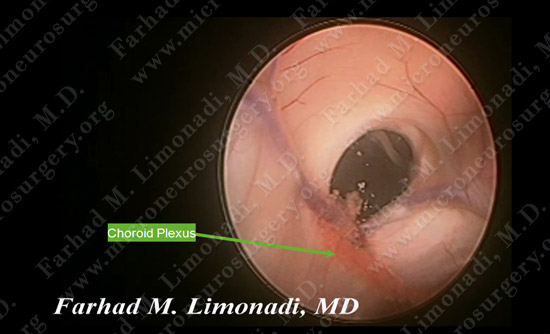
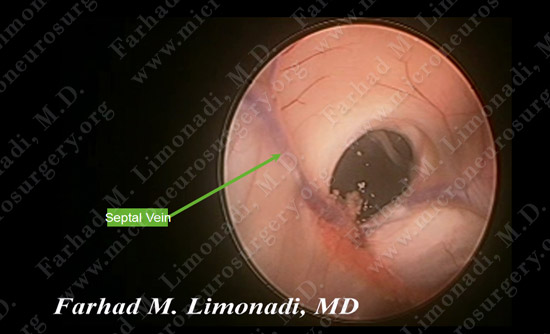
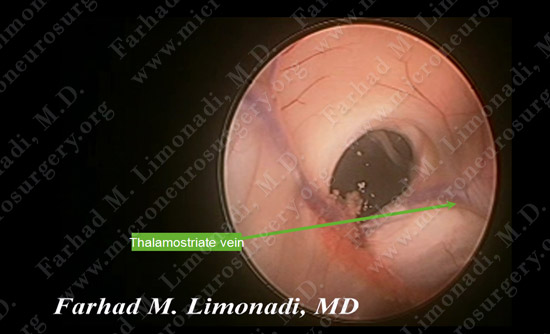
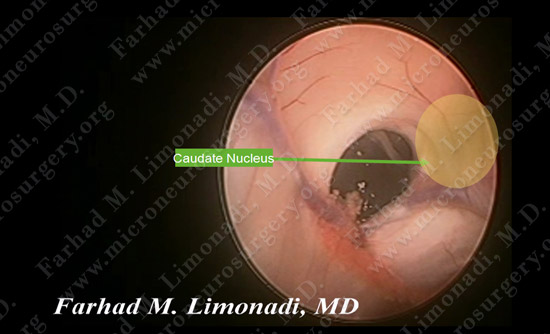
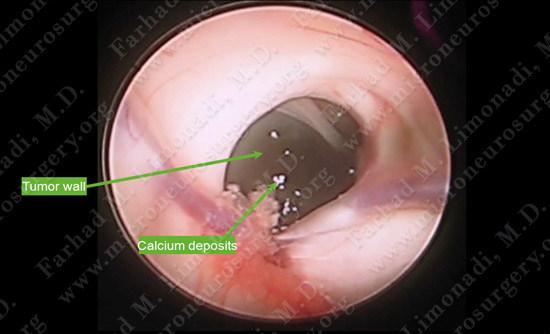
As then neuro-endoscope is driven closer to the forman of Monro, the shining wall of the tumor within the third ventricle becomes visible. Calcium deposition on the wall of the tumor is seen.
Neuro-endoscope is then carefully utilized to remove the tumor carefully from the third ventricle and follow the tumor into the peri-mesencephalic cistern and removing it around the basilar artery.
{loadposition Craniopharyngiomacase1}
Pathology
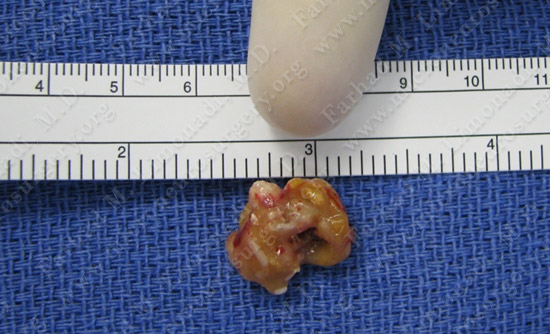
Tumor/Cyst Specimen which was sent for pathological review.

Post-op Course

Small incision was closed post-operatively.
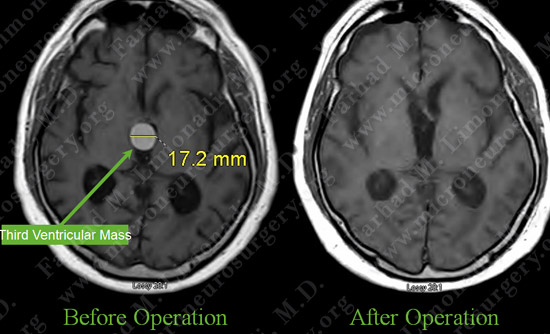
Post op MRI shows complete resection of the tumor with no injury to surrounding neuro-vascular structures. Most importantly patient had no neurological deficit after the operation.