Case Presentation:
Glioblastoma Multiforme (GBM) - Case 9
- Patient is a 60+ year old gentleman who was experiencing funny smells lasting a few minutes (olfactory hallucination secondary to uncinate seizure).
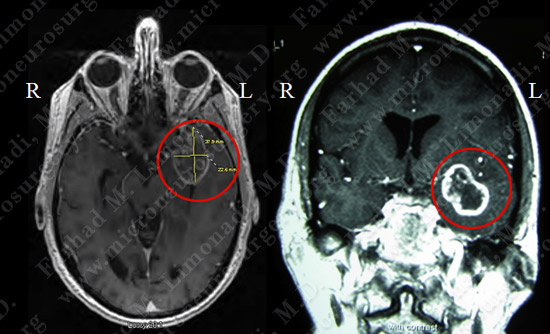
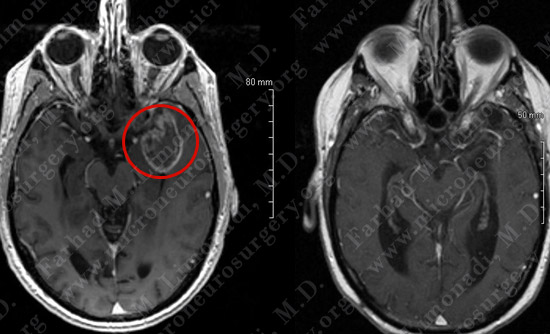
- He underwent a thorough evaluation by his neurologist including an MRI scan of the brain.
- On neurological examination, he had no deficit.
Imaging
Surgical Procedure
- Patient was prepared to undergo an awake craniotomy for gross total resection of the tumor.
- During this procedure patient undergoes general anesthesia and remains unconscious until the tumor is exposed. Then he is awakened and neurologically examined as the tumor is being removed carefully.


While patient is asleep, electrodes are attached to his scalp, arms and legs for intraoperative electrophysiological monitoring.
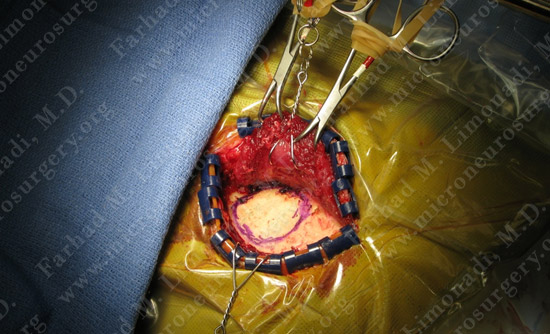
Left temporal bone is exposed and craniotomy margins are marked. Patient is under general anesthesia throughout this process.
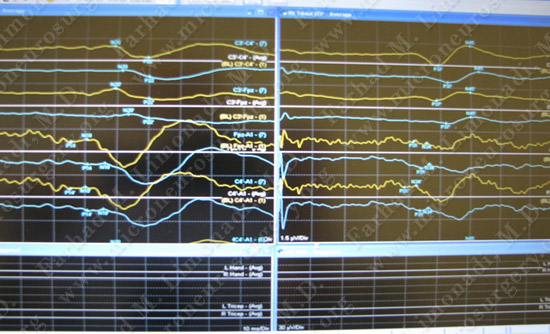
Patient’s SSEP and MEP are monitored during intraoperative neurophysiological assessment.
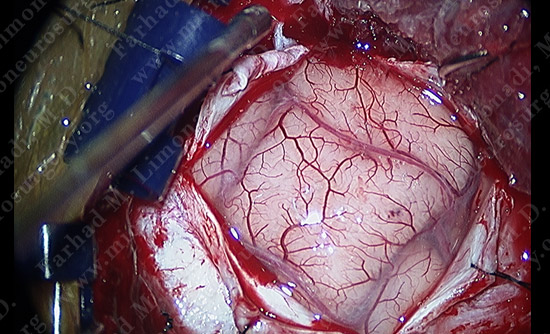
View through the surgical microscope shows the patient’s temporal lobe (brain) exposed. It is time to wake the patient up and proceed with resection of the tumor. It is important to note that the brain does not have pain receptors and the patient will not feel any pain.
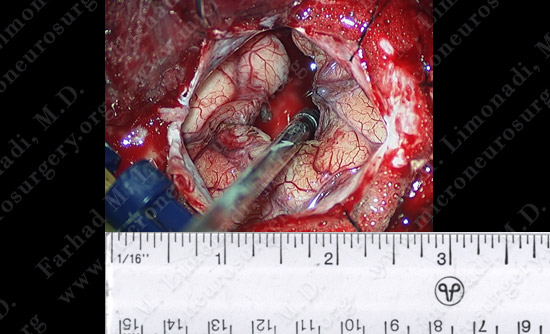
View through the surgical microscope shows the patient’s temporal lobe (brain) is exposed and the tumor is removed while he was awake and his speech was examined during the procedure.
Pathology
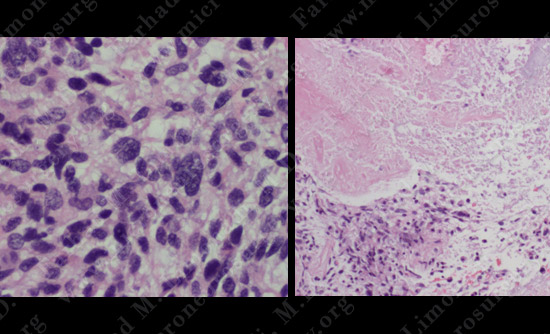
H&E slide of tumor Pleomorphic Astrocytes (left) and H&E slide of brain tumor zones of necrosis (right)
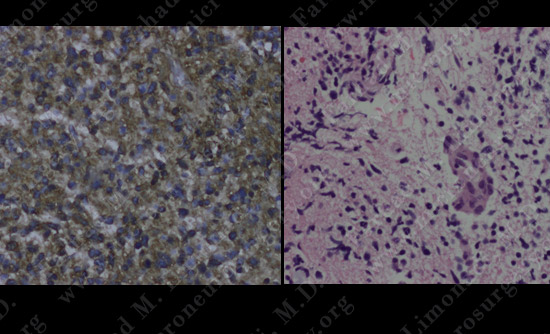
GFAP Stain Positive (left) and H&E slide of brain tumor Endothelial hyperplasia (right)
The pathology of the tumor suggested the diagnosis of glioblastoma multiforme (GBM).
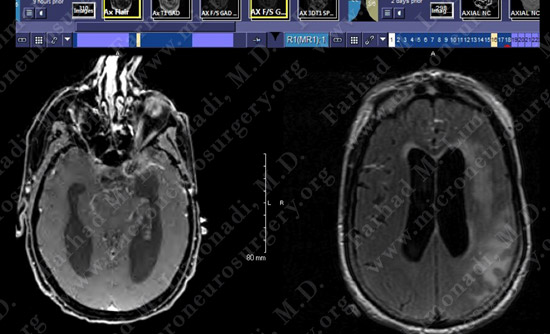
Post-op Imaging
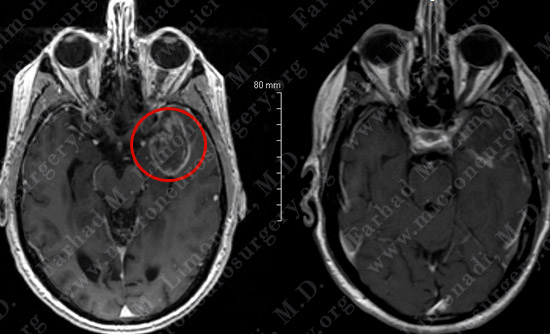
Before Operation After Operation
Post-op day 1 MRI shows complete resection of the tumor with no injury to surrounding neurovascular structures.
Post-op Course
- Patient did well postoperatively. He was discharged home and returned to full and normal function.
Post-op - 6 Months
Before Operation After Operation
At 6 months post-op patient was doing well and his team had won a competitive cognitive game. MRI shows no evidence of recurrence of the tumor by this time.
Post-op course - 18 Months
- Patient presented with headache, nausea and vomiting and altered mentation and became comatose.
- He was brought to the hospital promptly for evaluation.
- Seizure was ruled out via EEG.
- Due to wide dissemination of the tumor in the left cerebral hemisphere, patient was not a candidate for surgical resection of the tumor.
- He was treated with high dose steroids and ventriculostomy (as a temporary measure) which improved his neurological status.
- He was subsequently scheduled to undergo minimally invasive third ventriculostomy for treatment of obstructive hydrocephalus.
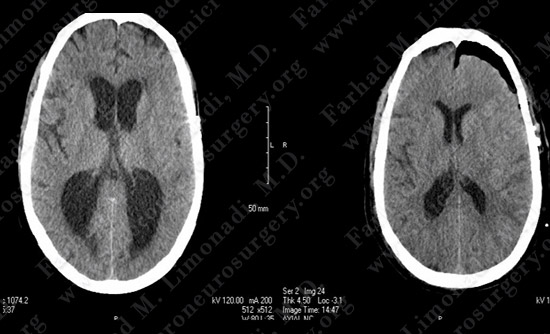
Current CT Post-op Day One
His CT scan demonstrated ventriculomegaly with evidence of obstructive hydrocephalus
MRI scan of the brain confirmed the CT finding and showed cerebral edema in left hemisphere due to tumor recurrence.
Surgical Procedure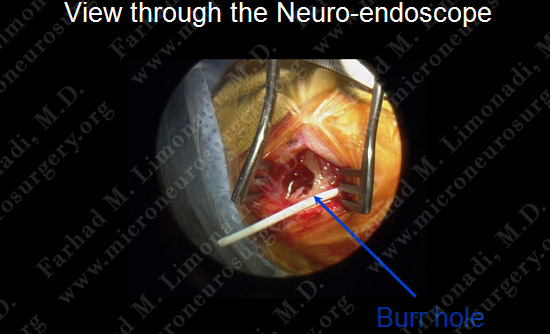
This operation was performed utilizing a small incision (one inch) and a small burr hole.
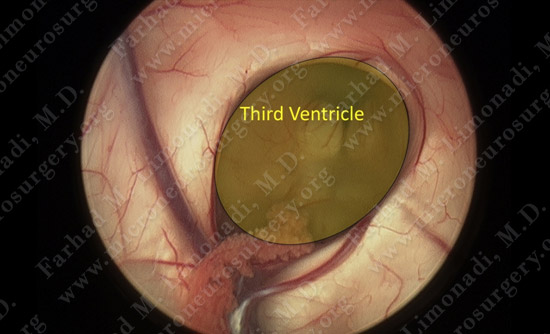
Upon entry into the fourth ventricle, the third ventricle can be seen through the foramen of Monro.
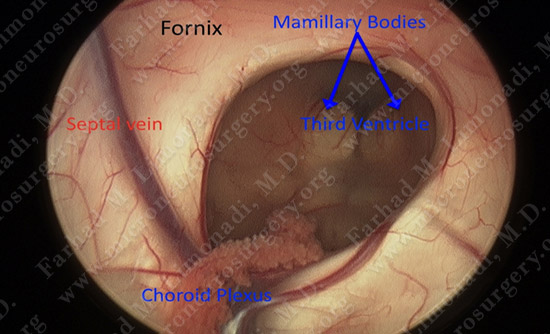
View through the Neuroendoscope.
Third ventriculostomy performed for treatment of obstructive hydrocephalus.
Post-op Course
- Upon successful third ventriculostomy patient did not require a VP shunt placement.
- Patient’s neurological status improved with following commands, oriented intermittently, and walking with physical therapy.